Abstract
Background
Little is known on whether there are ethnic differences in outcomes following percutaneous coronary intervention (PCI) and coronary artery bypass grafting surgery (CABG) after acute myocardial infarction (AMI). We compared 30-day and long-term mortality, recurrent AMI, and congestive heart failure in South Asian, Chinese and White patients with AMI who underwent PCI and CABG.
Methods
Hospital administrative data in British Columbia (BC), Canada were linked to the BC Cardiac Registry to identify all patients with AMI who underwent PCI (n = 4729) or CABG (n = 1687) (1999–2003). Ethnicity was determined from validated surname algorithms. Logistic regression for 30-day mortality and Cox proportional-hazards models were adjusted for age, sex, socio-economic status, severity of coronary disease, comorbid conditions, time from AMI to a revascularization procedure and distance to the nearest hospital.
Results
Following PCI, Chinese had higher short-term mortality (Odds Ratio (OR): 2.36, 95% CI: 1.12-5.00; p = 0.02), and South Asians had a higher risk for recurrent AMI (OR: 1.34, 95% CI: 1.08-1.67, p = 0.007) and heart failure (OR 1.81, 95% CI: 1.00-3.29, p = 0.05) compared to White patients. Risk of heart failure was higher in South Asian patients who underwent CABG compared to White patients (OR (95% CI) = 2.06 (0.92-4.61), p = 0.08). There were no significant differences in mortality following CABG between groups.
Conclusions
Chinese and South Asian patients with AMI and PCI or CABG had worse outcomes compared to their White counterparts. Further studies are needed to confirm these findings and investigate potential underlying causes.
Similar content being viewed by others
Background
Coronary revascularization including percutaneous coronary intervention (PCI) and coronary artery bypass graft (CABG) surgery, is among the most common and most expensive major medical procedures provided in North America [1], and is recommended by national guideline bodies for the management of selected patients with acute myocardial infarction (AMI) [2, 3]. Percutaneous coronary intervention has been shown to be more effective than thrombolytic therapy for reperfusion [2, 4]. In patients with AMI whose coronary anatomy appears unsuitable for PCI, CABG [3] or conservative treatment is indicated.
As burden of coronary heart disease has been increasing in developing countries such as India and China [5, 6], use of coronary revascularization technology will likely rise globally. However, there is little evidence on the effectiveness of these procedures in South Asian and Chinese populations with AMI and how it compares to White population. Although no studies explored the ethnic differences in outcomes in the post-AMI post-revascularization setting, in patients with coronary artery disease who have undergone revascularization procedures, studies yielded conflicting results. Namely, while some studies reported no difference in mortality rates following PCI between South Asian and White patients [7, 8], other observed lower mortality among Asian patients compared to their Western European counterparts [9]. Similarly, among studies exploring the ethnic differences in fatal cardiac outcomes following CABG, some studies reported higher mortality in South Asian compared to White patients [10–12], while others observed no such difference [13]. However, these studies are limited by lack of adjustment for differences in baseline prognostic characteristics, some by small sample sizes, and the effectiveness of revascularization is known to differ between AMI populations and those with stable coronary artery disease [2, 14]. Therefore, the objective of this analysis was to evaluate ethnic differences in fatal and non-fatal outcomes following PCI and CABG in Chinese, South Asian, and White patients who have suffered acute myocardial infarction (AMI) while controlling the analyses for potential confounders such as socio-demographics, severity of coronary artery disease, and presence of comorbid conditions.
Methods
Data sources
For this retrospective cohort study, data were derived from the hospital administrative data collected in the province of British Columbia (BC), Canada, and the BC Cardiac Registry from April 1999 to March 2003. The hospital administrative data include demographics, admission and discharge dates, and most responsible diagnosis for admission along with comorbid conditions for all patients admitted to hospital in BC. The BC Cardiac Registry data include the type, date and clinical details of the revascularization procedure performed, data on the indication for the procedure, extent of coronary artery disease, complications and other outcomes. The Registry includes all such procedures performed in the province. The Vital Statistics file contains the date of death for all patients with legislated mandatory reporting and is updated daily. Data were linked using a unique identifier common to all databases.
Study population
All patients with AMI diagnosed 1999–2003 in BC were identified using a validated coding algorithm in the hospital administrative database [15] based on the most responsible diagnosis code (International Classification of Diseases, ninth revision [ICD 9], 410.x). This coding algorithm has a positive predictive value of 95% (91% to 98%) identifying the physician’s diagnosis of acute myocardial infarction from hospital charts [16]. Patients younger than 20 years of age and those who were discharged from hospitalized for less than one day were excluded from the study to reduce the risk of false-positive diagnosis of AMI.
Revascularization and outcomes
For the study primary end-points, short (30-day) and long-term mortality, date of death was obtained from the BC Vital Statistics file. The secondary end-points included first recurrence of AMI and readmission to the hospital for heart failure (ICD 9, 428.x), and these were derived from hospital administrative data. For the study end-points, patients were followed-up for a maximum of 4 years.
Other prognostic variables
To adjust for baseline prognostic differences between groups, we used the mortality prediction rule following AMI [17] that was validated for 30-day and 1-year mortality displaying reasonable accuracy (areas under the curve was 0.78 and 0.79 for 30-day and 1-year mortality, respectively). The variables included age (dichotomized into 20–64 and 65 years of age and older), sex, area-level socio-economic status (assessed from area-level median household income based on the 2001 Canadian Census), and presence of comorbid conditions such as heart failure, cardiogenic shock, arrhythmia (any atrial or ventricular arrhythmia), diabetes mellitus, cerebrovascular disease, cancer, and acute or chronic renal disease. We also determined distance to the nearest hospital (defined as distance between the postal code centroids of the residential area and the nearest hospital), duration from diagnosis of AMI to revascularization procedure examined in the model, and severity of coronary artery disease based on Duke Criteria [18, 19].
Defining ethnicity
Ethnicity data were not available in administrative data. The Nam Pehchan computer program [20] and Chinese surname list [21] were used to identify study participants of South Asian and Chinese ethnicity, respectively. According to the 2006 Canadian Census, in British Columbia Canadian province, South Asians and Chinese were the two largest visible minority groups, while the remaining population was predominantly White [22]. Consequently, the rest of the study non-South Asian and non-Chinese participants were classified as White. Nam Pehchan program has been shown to classify South Asian names with 90.5% sensitivity and 99.4% specificity, while a positive predictive value of the program was 63.2% [20]. Sensitivity, specificity and a positive predictive value of the Chinese surname list are 77.7%, 99.7%, and 80.5% respectively [21]. In the event of changing surnames following an interracial marriage, misclassification may occur; however, using Chinese surname list, there was only a small drop in sensitivity when married females (Sensitivity = 73.2%) were compared to never-married ones (76.7%). In addition, validation of Nam Pehchan program revealed only 0.05% of the 356,555 names to have mixed components of South Asian and non-South Asian origins [20].
Statistical analysis
Ethnic differences in baseline characteristics were tested using Chi-square test or Fisher’s exact test, where appropriate. Ethnic differences in short-term mortality (up to 30 days after AMI) were modeled using logistic regression. Furthermore, ethnic differences in long-term mortality (30 days to a maximum of 4 years after index AMI), time to the first recurrent AMI, and hospitalization for heart failure were evaluated using Cox proportional-hazards modeling. The proportional hazard assumption was assessed using the methods based on cumulative sums of martingale residuals [23]. Firth correction methods were applied in the regression models in case of monotone likelihood with infinite estimates [24, 25]. All regression models were adjusted for age, sex, socio-economic status, distance to the nearest hospital, duration from the diagnosis of AMI to a revascularization procedure examined in the model, severity of coronary disease and presence of comorbid conditions (congestive heart failure, cardiogenic shock, arrhythmia, diabetes mellitus, cerebrovascular disease, cancer, and acute or chronic renal disease) based on the Ontario AMI mortality prediction rule [17]. Analyses were performed using SAS statistical software version 9.1 (SAS Institute Inc., Cary, NC). The University of British Columbia institutional research ethics board approved the study.
Results
Baseline characteristics
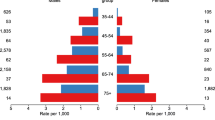
Out of 6416 patients with AMI who underwent revascularization, 2.8% were Chinese, 8% were South Asian and 89.2% were White patients. By the revascularization procedure, out of 4729 patients with AMI who underwent PCI, 3% were Chinese, 7.8% were South Asian and 89.2% were White patients. Furthermore, 1687 patients underwent CABG within one year of AMI out of which 2.6% were Chinese, 8.1% South Asian and 89.3% were White patients. Among those who underwent PCI (Table 1), South Asian patients were younger at the time of AMI presentation compared to Chinese and White patients. Diabetes mellitus was more prevalent among South Asian patients, followed by Chinese and White patients. Chinese were more likely to have hypertension compared to their South Asian and White counterparts. Further, the prevalence of cerebrovascular disease and cardiac dysrhythmias was highest among Chinese and lowest among South Asian patients.
As outlined in Table 2, similar to the PCI population, among patients who underwent CABG, South Asian patients were younger at AMI presentation and more likely to have diabetes mellitus compared to their Chinese and White counterparts. However, the prevalence of cardiogenic shock was highest among Chinese patients, followed by South Asian and White patients. The highest prevalence of 3-vessel coronary artery disease was among South Asians, followed by White and Chinese patients.
Outcomes
One hundred and sixteen patients died within 30 days from PCI (6.5% of Chinese patients (n = 9), 3.0% of South Asian (n = 11), and 2.3% of White patients (n = 96)). Within a year from PCI, there were 23, 16, and 23 fatalities per 1000-patient years in Chinese, South Asian and White patients, respectively. Among those who underwent CABG within 30 days following AMI, 4.7% of Chinese (n = 2), 2.2% of South Asians (n = 3), and 4.1% of White patients (n = 62) died. With regards to long-term mortality following CABG, there were 0, 30 and 21 events per 1000-patient years in Chinese, South Asian and White patients, respectively. After controlling for baseline characteristics, the odds of short-term mortality were significantly higher among Chinese compared to White patients who underwent PCI (Table 3). In the adjusted analyses, the risk of recurrent AMI and heart failure was found to be higher among South Asian than in White patients following PCI. No other ethnic differences were noted among patients who underwent PCI. Among patients who underwent CABG, there were no statistically significant ethnic differences in mortality and risk of recurrent AMI, however, the risk of heart failure was significantly higher among South Asian patients than in White patients.
Discussion
In this observational study we found significantly worse prognosis in South Asian and Chinese patients with AMI following revascularization compared to their White counterparts. These observed ethnic differences in mortality, risk of recurrent AMI, and heart failure were independent of age, sex, socio-economic status, distance to the nearest hospital, the duration from an AMI diagnosis to a revascularization procedure, severity of coronary disease and comorbid conditions.
Our findings of higher short-term mortality among Chinese patients following PCI are in contrast to those of a recent study where the rates of all-cause and cardiac mortality following PCI were lower in Asian patients (Singapore, Hong Kong, and Malaysia) compared to their counterparts from Western Europe [9]. This difference may be due to the fact that our population was an AMI population compared to a lower risk unselected coronary disease population in the study above. Moreover, we directly compared outcomes in ethnic groups within a single health care system whereas Klomp et al. indirectly compared patients in differing health care systems [9, 26].
Higher short-term mortality following PCI among Chinese patients compared with their White counterparts may have occurred for several reasons. Chinese patients may have had arrived later to the emergency department [27, 28] resulting in less effectiveness of the procedures or more extensive myocardial damage at time of PCI [29]. However, in our study, we extensively adjusted for differences in baseline prognostic characteristics and extent of coronary disease. Chinese patients may also have had higher post procedural complications or differences in coronary artery disease management. Chinese patients have been shown to have a lower rate of filling their prescriptions and for adhering to secondary prevention medications [30, 31]. Furthermore, they have a greater use of herbal medications [32]. In addition, there may be genetic differences in antiplatelet responsiveness between the ethnic groups [33, 34] placing Chinese patients at higher risk of peri- and post procedural complications.
While no difference between South Asian and White patients was observed for mortality, South Asian patients were found to be at greater risk of non-fatal adverse cardiovascular events following PCI and CABG compared with White patients, even when examining survivors only. Other studies examining ethnic differences in outcomes following PCI or CABG have reported conflicting results. While several studies of unselected coronary disease patients have revealed no difference in fatal cardiac outcomes between South Asian and White patients following PCI [7, 8] and CABG [13], others have observed higher CABG postoperative mortality in South Asian than in White patients [10–12]. However, the latter studies did not adjust for prognostic factors that may have contributed to the conflicting results and did not directly study AMI populations.
Our study represents a direct comparison of ethnic differences of AMI patients in a single health care system using extensive adjustment for prognostic factors including severity of coronary disease. However, several study limitations should be noted. First, this study is an observational study and the ideal study design for determining efficacy of these procedures following AMI would be a randomized trial. This study is thus susceptible to treatment-selection bias and bias from residual confounding. Although we did adjust for multiple potential confounding factors, we were not able to control for risk behaviors (such as smoking, physical activity or diet), dyslipidemia or extent of infarct (non-ST elevation MI, or peak cardiac enzyme level) that could explain the observed difference in outcomes. Second, ethnicity was defined using surname algorithms because self-reported ethnicity data were not available. However, surname algorithms have been shown to have high sensitivity and specificity; however, there is a possibility that some of the ethnic categories were misclassified that could potentially underestimate inter-ethnic differences in study outcomes. Additionally, we did not know generational status of patients, but likely, given the age of patients in the cohort, most patients would be first generation immigrants.
Conclusions
This observational study found a worse prognosis in South Asian and Chinese patients following revascularization compared to their White counterparts. Observed ethnic disparities in outcomes were present despite adjustment for demographic, socio-economic and clinical characteristics. We believe that the availability of interpretation and translation services, the presence of education programs teaching the importance of adherence to secondary prevention medication, the recognition of early signs of AMI and timely seek of care, along with equitable access to health care, may help reduce ethnic disparities in postrevascularization outcomes. In addition, given the inter-ethnic differences in the response to clopidogrel antiplatelet therapy, a future personalized approach to therapy may further reduce the disparity in postrevascularization outcomes.
References
Mark DB, Hlatky MA: Medical economics and the assessment of value in cardiovascular medicine: part II. Circulation. 2002, 106: 626-630. 10.1161/01.CIR.0000021408.40925.63.
Kushner FG, Hand M, Smith SC, King SB, Anderson JL, Antman EM, Bailey SR, Bates ER, Blakenship JC, Casey DE, Green LA, Hochman JS, Jacobs AK, Krumholz HM, Morrison DA, Ornato JP, Pearle DL, Peterson ED, Sloan MA, Whitlow PL, Williams DO: 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update). A report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guideline. JACC. 2009, 54: 2205-2241. 10.1016/j.jacc.2009.10.015.
Steg G, James SK, Atar D, Badano LP, Blomstrom-Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez-Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, van’t Hof A, Widimsky P, Zahger D: ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force on the management of ST-segment elevation acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012, 33: 2569-2619.
Keeley EC, Boura JA, Grines CL: Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003, 361: 13-10.1016/S0140-6736(03)12113-7.
Gupta R, Joshi P, Mohan V, Reddy KS, Yusuf S: Epidemiology and causation of coronary heart disease and stroke in India. Heart. 2008, 94: 16-26. 10.1136/hrt.2007.132951.
Zhang X-H, Lu ZL, Liu L: Coronary heart disease in China. Heart. 2008, 94: 1126-1131. 10.1136/hrt.2007.132423.
Toor IS, Jaumdally R, Lip GYH, Pagano D, Dimitri W, Millane T, Varma C: Differences between South Asians and White Europeans in five year outcome following percutaneous coronary intervention. Int J Clin Pract. 2011, 65: 1259-1266. 10.1111/j.1742-1241.2011.02776.x.
Jones DA, Rathod KS, Sekhri N, Junghans C, Gallagher S, Rothman MT, Mohidin S, Kapur A, Knight C, Archbold A, Jain AK, Mills PG, Uppal R, Mathur A, Timmis AD, Wragg A: Case death rates for South Asian and Caucasian patients show no difference 2.5 years after percutaneous coronary intervention. Heart. 2012, 98: 414-419. 10.1136/heartjnl-2011-300130.
Klomp M, Damman P, Beijk MAM, Tan KH, Balian V, de Luca G, Tijssen JGP, Silber S, de Winter RJ, on behalf of the e-HEALING investigators: Differences in cardiovascular risk factors and clinical outcomes between Western European and Southeast Asian patients treated with the Genous Bio-engineered R stent: an e-HEALING wordwide registry substudy. Coron Artery Dis. 2012, 23: 271-277. 10.1097/MCA.0b013e328351aaed.
Zindrou D, Peder Bagger J, Smith P, Taylor KM, Ratnatunga CP: Comparison of operative mortality after coronary artery bypass grafting in Indian subcontinent Asians versus Caucasians. Am J Cardiol. 2001, 88: 313-316. 10.1016/S0002-9149(01)01651-4.
Brister SJ, Hamdulay Z, Verma S, Maganti M, Buchanan MR: Ethnic diversity: South Asian ethnicity is associated with increased coronary artery bypass grafting mortality. J Thorac Cardiovasc Surg. 2007, 133: 150-154. 10.1016/j.jtcvs.2006.05.068.
Hadjinikolaou L, Klimatsidas M, Iacona GM, Spyt T, Samani NJ: Short- and medium-term survival following coronary artery bypass surgery in British Indo-Asian and white Caucasian individuals: impact of diabetes mellitus. Interact Cardiovasc Thorac Surg. 2010, 10: 389-393. 10.1510/icvts.2009.210567.
Goldsmith I, Lip GYH, Tsang G, Patel RL: Comparison of primary coronary artery bypass surgery in a British Indo-Asian and white Caucasian population. Eur Heart J. 1999, 20: 1094-1100. 10.1053/euhj.1998.1450.
Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, Knudtson M, Dada M, Casperson P, Harris CL, Chaitman BR, Shaw L, Gosselin G, Nawaz S, Title LM, Gau G, Blaustein AS, Booth DC, Bates ER, Spertus JA, Berman DS, Mancicni GBJ, Weintraub WS for the COURAGE Trial Research Group: Optimal medical therapy with or without PCI for stable coronary disease. NEJM. 2007, 356: 1503-1516. 10.1056/NEJMoa070829.
Tu JV, Austin PC, Naylor CD, Iron K, Zhang H: Acute myocardial infarction outcomes in Ontario. Cardiovascular health and services in Ontario: an ICES atlas. Edited by: Naylor CD, Slaughter PM. 1999, Toronto, Ontario: Institute for Clinical Evaluative Sciences, 83-110.
Varas-Lorenzo C, Castellsague J, Stang MR, Tomas L, Aguado J, Perez-Gutthann S: Positive predictive value of ICD-9 codes 410 and 411 in the identification of cases of acute coronary syndromes in the Saskatchewan Hospital automated database. Pharmacoepidemiol Drug Saf. 2008, 17 (8): 842-852. 10.1002/pds.1619.
Tu JV, Austin PC, Walld R, Roos L, Agras J, McDonald KM: Development and validation of the Ontario acute myocardial infarction mortality prediction rules. JACC. 2001, 37: 992-997. 10.1016/S0735-1097(01)01109-3.
Bart BA, Shaw LK, McCants CB, Fortin DF, Lee KL, Califf RC, O’Connor CM: Clinical determinants of mortality in patients with angiographically diagnosed ischemic or nonischemic cardiomyopathy. JACC. 1997, 30: 1002-1008. 10.1016/S0735-1097(97)00235-0.
Liao L, Kong DF, Shaw LK, Sketch MH, Milano CA, Lee KL, Mark DB: A new anatomic score for prognosis after cardiac catheterization in patients with previous bypass surgery. JACC. 2005, 46: 1684-1692. 10.1016/j.jacc.2005.06.074.
Cummins C, Winter H, Cheng K, Maric R, Silcocks P, Varghese C: An assessment of the Nam Pehchan computer program for the identification of names of South Asian ethnic origin. J Public Health Med. 1999, 21: 401-406. 10.1093/pubmed/21.4.401.
Quan H, Wang F, Schopflocher D, Norris C, Galbraith D, Faris P, Graham MM, Knudtson ML, Ghali WA: Development and validation of a surname list to define Chinese ethnicity. Med Care. 2006, 44: 328-333. 10.1097/01.mlr.0000204010.81331.a9.
Statistics Canada 2: Ethnic groups and generation in Canada. http://www5.statcan.gc.ca/subject-sujet/result-resultat.action?pid=30000&id=30002&lang=eng&type=CST&pageNum=1&more=0,
Lin DY, Wei LJ, Ying Z: Checking the Cox model with cumulative sums of martingale-based residuals. Biometrika. 1993, 80: 557-572. 10.1093/biomet/80.3.557.
Heinze G, Schemper M: A solution to the problem of monotone likelihood in Cox regression. Biometrics. 2001, 57: 114-119. 10.1111/j.0006-341X.2001.00114.x.
Heinze G, Schemper M: A solution to the problem of separation in logistic regression. Stat Med. 2002, 21: 2409-2419. 10.1002/sim.1047.
Gupta M, Chang W-C, Van der Werf F, Granger CB, Midodzi W, Barbash G, Pehrson K, Oto A, Toutouzas P, Jansky P, Armstrong PW, for the ASSENT II investigators: International differences in in-hospital revascularization and outcomes following acute myocardial infarction. A multilevel analysis of patients in ASSENT-2. Eur Heart J. 2003, 24: 1640-1650. 10.1016/S0195-668X(03)00433-0.
King KM, Khan NA, Quan H: Ethnic variation in acute myocardial infarction presentation and access to care. Am J Cardiol. 2009, 103: 1368-1373. 10.1016/j.amjcard.2009.01.344.
Heron SL, Stettner E, Haley LL: Racial and ethnic disparities in the emergency department: a public health perspective. Emerg Med ClinNorth Am. 2006, 24: 905-923.
Ayanian JZ: Diversity in cardiovascular outcomes among Chinese and South Asian patients. Circulation. 2010, 122: 1550-1552. 10.1161/CIRCULATIONAHA.110.982058.
Morgan S, Hanley G, Cunningham C, Quan H: Ethnic differences in the use of prescription drugs: a cross-sectional analysis of linked survey and administrative data. Open Med. 2011, 5: e87-e92.
Lai EJ, Grubisic M, Palepu A, Quan H, King KM, Khan NA: Cardiac medication prescribing and adherence after acute myocardial infarction in Chinese and South Asian Canadian patients. BMC Cardiovasc Disord. 2011, 11: 56-10.1186/1471-2261-11-56.
Quan H, Lai D, Johnson D, Verhoef M, Musto R: Complimentary and alternative medicine use among Chinese and white Canadians. Can Fam Physician. 2008, 54: 1563-1569.
Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT, Walker JR, Antman EM, Macias W, Braunwald E, Sabatine MS: Cytochrome P-450 polymorphisms and response to clopidogrel. NEJM. 2009, 360: 354-362. 10.1056/NEJMoa0809171.
Chan MY: Clopidogrel pharmacokinetics of east, south and other Asian populations. Eur Heart J Suppl. 2012, 14 (SupplA): A41-A42.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2261/13/121/prepub
Acknowledgements
This study was funded by the Canadian Institutes for Health Research.
AFA receives salary support from the Cardiac Services of British Columbia and Provincial Health Services Authority for a special grant for South Asian cardiovascular health initiative. NAK receives salary support from the Michael Smith Foundation for Health Research Career Scientist Award. HQ receives salary support from the Alberta Heritage Foundation for Medical Research Senior Population Investigator award. MM is supported by a Heart and Stroke Foundation of Canada Research Scholarship. We thank the Ministry of Health for British Columbia and the British Columbia Cardiac Registry Services for providing access to the research data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare no competing interests.
Authors’ contributions
DG participated in the design of the study, interpreted the data and drafted the manuscript. NAK made substantial contributions to design of the study and data interpretation, helped to draft the manuscript, and she critically revised it. HQian performed statistical analyses and contributed to data interpretation. SK participated in the discussion and critically revised the manuscript. GS contributed to the conception of the study, participated in the discussion and critically revised the manuscript. HQuan participated in the discussion and critically revised the manuscript. MHM participated in the discussion and critically revised the manuscript. BJO participated in the discussion and critically revised the manuscript. AFA conceived the study, participated in its design, data interpretation, the manuscript discussion and critically revised the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Gasevic, D., Khan, N.A., Qian, H. et al. Outcomes following percutaneous coronary intervention and coronary artery bypass grafting surgery in Chinese, South Asian and white patients with acute myocardial infarction: administrative data analysis. BMC Cardiovasc Disord 13, 121 (2013). https://doi.org/10.1186/1471-2261-13-121
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2261-13-121